Mr Rahul Patel, a consultant knee surgeon at London Bridge Orthopaedics, discusses hip arthroscopy and femoroacetabular impingement (FAI) and the most recent developments in diagnostics and outcomes.
With the ongoing explosion in hip arthroscopy procedures worldwide, patients are being referred in increasing numbers for the evaluation of hip pain. Many of these patients engage in athletic activity and are understandably unwilling to limit their activity. As a result, the understanding of the functional anatomy of this anatomical area has been improved and refined. Concurrently, the advancement of MRI has enabled the diagnosis of soft tissue causes of hip and groin pain to be greatly enhanced. Consequently, the differential diagnosis of hip pain has been broadened and treatment vastly improved.
Historically, hip pain was treated with prolonged conservative management and activity restriction. Open procedures were considered if they failed but with the advent of hip arthroscopy the landscape has been changed; large numbers of patients are enjoying the advantages of arthroscopic treatment and returning to their full activities quickly.
It is best to think of the causes of hip pain as intra-articular, extra-articular and disorders that cause groin pain (table 1, below). There is of course considerable overlap between groin disorders that cause groin pain and intra-articular pathology which also causes groin pain, hence the diagnostic challenge! Arthroscopy can be used to treat both intra- and extra-articular causes but not all of them.
Causes of pain around the hip joint
PLAC – Pyramidalis – anterior pubic Ligament – Adductor longus Complex
RA/AL – Rectus Abdominis / Adductor Longus
| Intra-articular |
Extra-articular |
Groin disorders |
| Femoroacetabular impingement |
Iliopsoas tendinopathy |
Athletic pubalgia (PLAC, RA/AL aponeurosis tear) |
| Labral tears |
Iliotibial band syndrome |
Pubic bone overload |
| Loose bodies |
Trochanteric bursitis |
Obturator neuropathy |
| Ligamentum teres rupture |
Gluteus medius/minimus tendinosis |
Pubic symphysis dysfunction (incl. degeneration) |
| Chondral damage |
Piriformis syndrome |
|
| Capsular laxity |
Stress fracture |
|
| Developmental dysplasia |
Adductor strain |
|
|
Sacroiliac joint pathology |
|
What is Femoro-acetabular impingement?
Femoro-acetabular impingement (FAI) has received significant attention as it has now been established that it is a cause of hip joint osteoarthritis in some patients. Therefore, early diagnosis and treatment of this condition might prevent or delay the onset of osteoarthritis. Put simply, FAI is an abutment conflict between the bone of the femur and that of the pelvis.
The causes of impingement in the hip can be linked to childhood hip disorders (Perthes, slipped upper femoral epiphysis) or can arise from post-traumatic or post-osteotomy changes in structural anatomy. However, the vast majority of cases remain idiopathic, but theories exist around the subjects of genetic predisposition and activity-related modelling of the hip joint during childhood and adolescence.
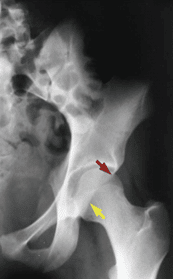
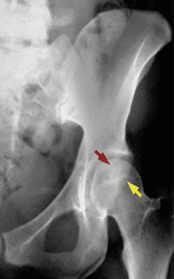
Three main types of impingement (figure 1, below) have been described: CAM impingement results from abnormalities at the femoral head-neck junction impacting the acetabulum causing labral and chondral damage (more common in young males). Pincer impingement results from acetabular over-coverage (e.g., acetabular retroversion (figure 2, below), coxa profunda or protrusio), resulting in impingement of a normal femoral head-neck junction on the acetabular rim (more common in middle-aged females). The mixed form is a combination of the two, thought to be the commonest. Approximately 25% of the population are thought to demonstrate radiographic features of FAI but only 5-10% are symptomatic. Bilaterality of radiographic features does not necessarily equate to bilateral symptoms.

Figure 1 (above). Biomechanics of hip impingement seen on an axial view of the hip joint.
A: Normal hip. B: CAM. C: PINCER- excessive over-coverage of femoral head D: Combined.
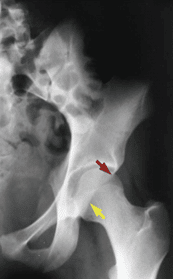
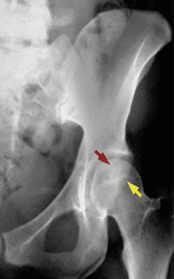
Figure 2 (above). Red arrow indicates the anterior acetabular wall and the yellow arrow indicates the posterior acetabular wall. Left: this is the normal relationship in an anteverted acetabulum. Right: Note the “crossover” of the wall margins: acetabular retroversion
Each type causes repetitive microtrauma to the labrum and/or articular cartilage resulting in distinct patterns of injury. In pincer impingement, an indentation at a normal femoral head-neck junction caused by repeated abutment against the anterior acetabular margin and an ossified labrum is seen.
The shear forces in CAM impingement produce an outside-in abrasion of the acetabular cartilage and/or its avulsion from the labrum and the subchondral bone in the anterosuperior rim area. Arthritis develops when damage at the labral-cartilage junction extends to the articular cartilage and subchondral bone.
What are the Clinical features of FAI?
A young or middle-aged patient who describes the gradual onset of unilateral hip pain that is predominantly in the anterolateral thigh or groin must be considered to have femoroacetabular impingement. The patient may report mechanical symptoms (locking, catching) indicative of a labral tear or a delamination injury of the articular cartilage. The pain is often intermittent and exacerbated by excessive demand on hip flexion, such as occurs with athletic activities and in very flexible hips.
The most important physical finding is the result of the impingement test, which reveals limitations of internal rotation and adduction in flexion out of proportion with limitations of other motions. With the patient supine, the hip is internally rotated as it is passively flexed to approximately 90° and adducted. Flexion and adduction cause abutment of the femoral neck on the acetabular rim. Further passive internal rotation induces shear forces at the labrum and can create a sharp pain when there is a labral and/or a chondral lesion.
How is FAI Diagnosed?
Plain radiographs are the most important imaging studies for the diagnosis of FAI. The recommended radiographs are an anteroposterior view and cross-table lateral view of the hip in 15 degrees of internal rotation.
Further investigation using CT allows three-dimensional reconstruction of the hip joint for a detailed definition of femoral head-neck asphericities that cause osseous impingement as well as determination of the version of the femoral neck and acetabulum.
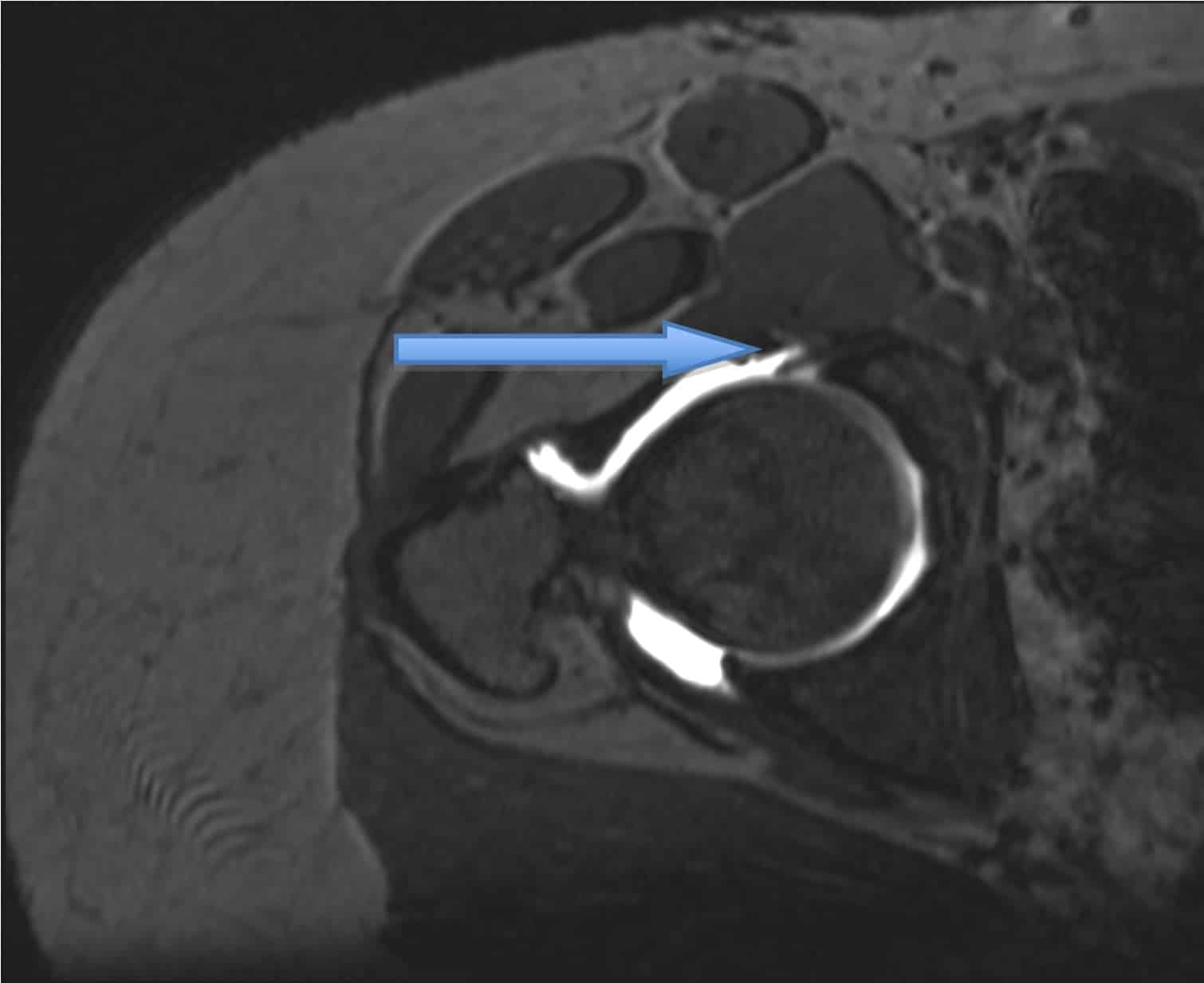
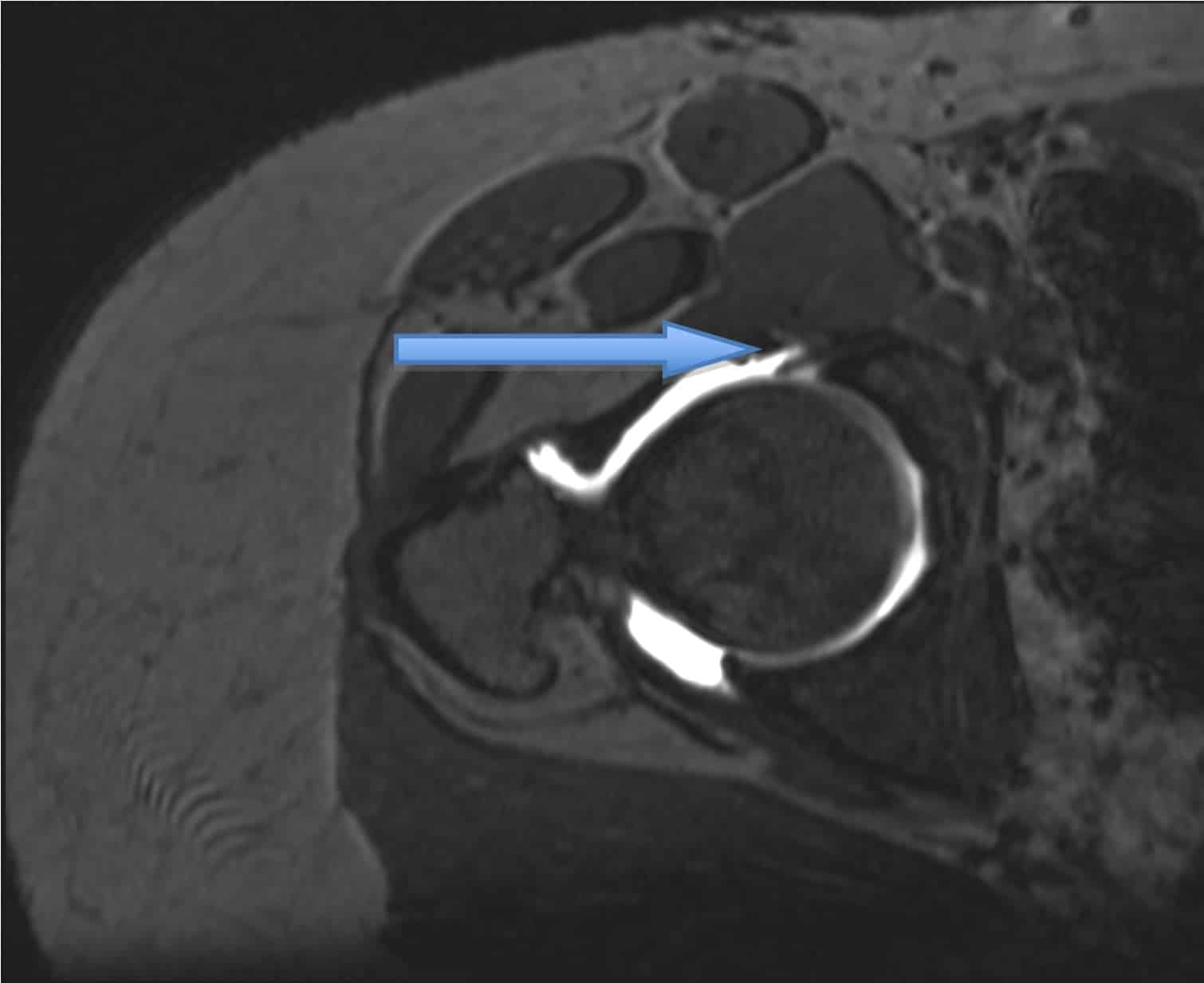
3T MRI is needed to assess labral (figure 3, below) and chondral injury as well as to demonstrate the contour of the femoral head-neck junction. In addition, MRI can exclude other causes of hip and groin pain.
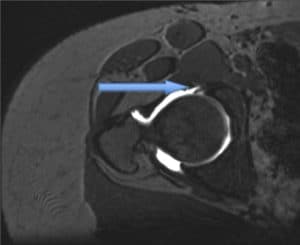
Figure 3 (above). MRI scan demonstrating labral tear.
The most useful diagnostic tool is a diagnostic injection, most often into the hip joint but occasionally targeted elsewhere under ultrasound guidance. The elimination of pain/symptoms temporarily provides confirmatory or exclusionary evidence for pathologies that are being considered.
Treatment options for FA
Non-operative
This may include modification of activity, restriction of athletic pursuits and reduction of excessive demand on the hip. Non-steroidal anti-inflammatory medication may relieve the pain. Physical therapy should emphasise muscle strengthening and avoidance of extremes of range of motion. The young age coupled with the high activity levels of these patients usually jeopardises compliance with non-operative treatment. Hip impingement is a mechanical problem and non-operative measures will not eliminate the patho-mechanics of structural deformities. However, physical therapy is eminently successful in the treatment of many of the other disorders listed above including instability and athletic pubalgia.
Operative
Operative treatment focuses on improving the clearance of hip motion and alleviating femoral abutment against the acetabular rim, which will relieve the pathological changes in the labrum and articular cartilage. Arthroscopy is becoming an increasingly popular method to treat FAI because of the obvious advantages of arthroscopic surgery and as technological advances are made to improve the specialised equipment, better outcomes are being achieved. However, if there is damage to the articular cartilage this may compromise the result of operative treatment. Thus, early diagnosis and treatment is paramount to success.
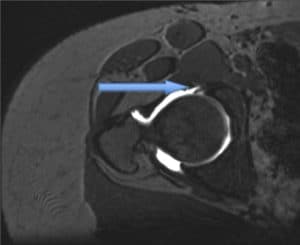
Arthroscopy (figure 4, below) essentially is divided into two phases: central compartment arthroscopy allows visualisation and treatment of articular surface and labrum pathologies including removal of loose bodies, labral repair, chondroplasty and microfracture; peripheral compartment arthroscopy refers to the femoral head-neck junction area where non-spherical aspects of the femoral head are corrected using high-speed burrs and shavers. Acetabular abnormalities can be addressed during either phase, commonly involving reducing bony over-coverage anteriorly using high-speed burrs.
Post-operatively, weight-bearing is usually restricted for 2 weeks to decrease the risk of a femoral neck fracture, but the use of stationary bicycles and swimming is encouraged thereafter. Most patients only require an overnight stay, and some centres manage the procedure as a day case.
The early results of hip arthroscopy are promising in terms of symptom and functional improvement. We have no knowledge yet of the ability of this operative technique to alter the course towards total hip replacement, but this will become apparent in time.

Figure 4 (above). Hip arthroscopy with instruments in anterior and anterolateral portals.
Summary
Patients with hip and groin pain can be a diagnostic headache; careful examination and investigation utilising a variety of modalities will usually reveal the pathology but can be time-consuming. FAI is one of the more common diagnoses seen and is usually excluded first by simple examination and radiology. Because FAI is believed to be a precursor to osteoarthritis, if it is suspected, early referral to a specialist is strongly recommended as early diagnosis and treatment using hip arthroscopy appears to yield promising outcomes.